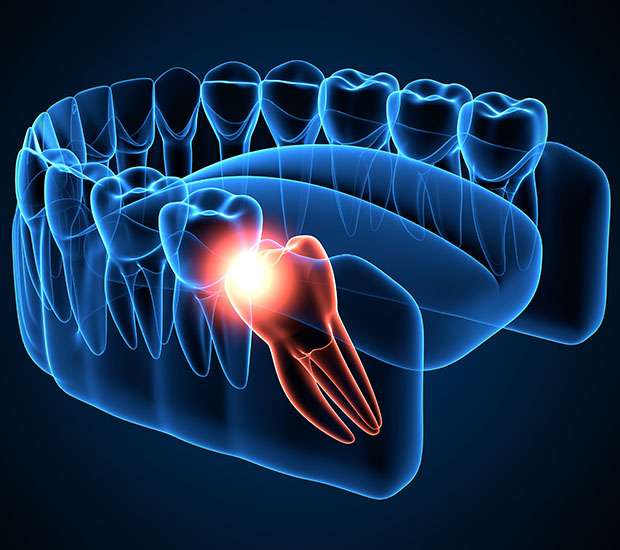
Wisdom teeth—also known as third molars—are the last teeth to erupt in the oral cavity and are often the first to require surgical intervention. While some erupt without issue, many become impacted, misaligned, or partially erupted, leading to a range of clinical problems.
For dental professionals, understanding the complexities of third molar extractions is essential—not only to improve patient outcomes but also to expand surgical competence and confidence in daily practice.
What Are Wisdom Teeth and Why Do They Often Need to Be Removed?
Wisdom teeth typically emerge between the ages of 17 and 25. However, due to evolutionary changes in jaw size and diet, many patients no longer have adequate space to accommodate these teeth properly. As a result, third molars often become:
- Impacted (trapped under bone or soft tissue)
- Misaligned (pushing into second molars or growing at an angle)
- Partially erupted (causing soft tissue infections)
Common indications for extraction include:
- Pain or swelling
- Pericoronitis (infection of soft tissue around a partially erupted tooth)
- Risk of caries in adjacent molars
- Orthodontic treatment planning
- Cyst formation or other pathology
Why Surgical Training in Third Molar Extractions Matters
Many general dentists refer out surgical extractions due to lack of training or confidence. However, with proper education and hands-on experience, third molar removal becomes a predictable and manageable procedure.
Clinical competence in third molar surgery enhances a dentist’s ability to:
- Perform extractions safely and efficiently
- Manage complications such as dry socket or infection
- Reduce dependency on referrals
- Improve patient care continuity
Key Components of Effective Wisdom Teeth Surgery
Performing a third molar extraction goes beyond simply “pulling a tooth.” It requires a structured surgical approach that includes:
-
Thorough patient assessment and radiographic analysis
Proper imaging (such as panoramic radiographs or CBCT) is critical for evaluating root position, angulation, and proximity to anatomical structures like the inferior alveolar nerve.
-
Flap design and soft tissue management
Creating an effective surgical flap allows access while preserving healing potential and reducing trauma.
-
Bone removal and odontosection
In complex cases, controlled removal of bone or sectioning of the tooth is required to minimize risk and facilitate removal.
-
Hemostasis and wound closure
Proper suturing techniques ensure optimal healing and reduce the chance of postoperative complications.
-
Postoperative care and complication management
Knowledge of pain management, infection control, and follow-up protocols is essential for ensuring good outcomes.
Training Opportunities for Dentists
The best way to develop these skills is through live patient training under expert supervision. A comprehensive hands-on program should offer:
- Real clinical cases from assessment to follow-up
- Supervised surgeries with personalized guidance
- Didactic instruction focused on technique, safety, and anatomy
- Complication management strategies for routine and complex cases
These programs allow dentists to bridge the gap between theory and practice, building confidence and skill in one of the most requested oral surgical procedures.
Final Thoughts
Wisdom teeth surgery is a cornerstone of oral surgical care. As patient demand grows and surgical expectations increase, dentists who are proficient in third molar extractions will be better equipped to deliver comprehensive, high-quality care.
Whether you’re a general practitioner looking to reduce referrals or a recent graduate aiming to build your surgical confidence, investing in third molar training is a critical step toward clinical growth.